Imagine you’re a man diagnosed with localized prostate cancer, a condition that affects approximately 1 in 9 men in the United States alone, according to the American Cancer Society. You’re faced with a daunting decision: which treatment path to take? Traditionally, radical prostatectomy (RP) has been the gold standard, but what if there’s a less invasive, equally effective alternative? This is where High-Intensity Focused Ultrasound (HIFU) comes into play, and the results of the HIFI trial have sparked a significant conversation in the urology community. Today, we delve into the fascinating world of HIFU vs radical prostatectomy, exploring the latest data that suggests noninferior treatment-free survival, and what this means for men and their families facing this challenging journey.
Agreeably, the thought of undergoing any cancer treatment is overwhelming. But what if you could potentially avoid the potential side effects of surgery, such as urinary incontinence and erectile dysfunction, without compromising your chances of survival? This is the promise that HIFU holds, and the HIFI trial outcomes have brought this possibility into sharper focus. The HIFI trial, a randomized, multicenter, open-label study, compared the efficacy of HIFU with that of RP in men with localized prostate cancer. The results, published in The Lancet, showed that HIFU was noninferior to RP in terms of salvage therapy-free survival, a metric that measures the time until a patient requires additional treatment due to cancer progression.
Now, you might be wondering, what does this mean for you or a loved one facing a prostate cancer diagnosis? In this article, we preview the key findings of the HIFI trial, explain the implications of these results in plain language, and guide you through the process of understanding your treatment options. We’ll also discuss the importance of informed decision-making and the role of a multidisciplinary healthcare team in your journey. By the end of this article, you’ll have a clearer understanding of HIFU vs radical prostatectomy, and you’ll be better equipped to navigate the complex world of prostate cancer treatment. So, let’s embark on this informative journey together, as we strive to empower you with the knowledge you need to make the best choice for your health and well-being.
HIFU vs Radical Prostatectomy: A New Hope for Prostate Cancer Patients
Prostate cancer, a common health concern among men, has traditionally been treated with invasive procedures like radical prostatectomy. This surgery, while effective, comes with potential side effects such as incontinence and impotence. However, a new hope has emerged in the form of High-Intensity Focused Ultrasound (HIFU).
HIFU is a minimally invasive treatment that uses focused ultrasound waves to heat and destroy prostate tissue. It offers several advantages over radical prostatectomy. Firstly, it’s an outpatient procedure, allowing patients to recover in the comfort of their own homes. Secondly, it has a lower risk of side effects, with many patients retaining their urinary and sexual function. Lastly, HIFU can be repeated if necessary, making it a viable option for recurrent prostate cancer.
While HIFU is not suitable for all prostate cancer patients, it’s a promising alternative for those with early-stage, localized disease. It’s crucial for men to discuss their treatment options with their healthcare provider, considering factors like cancer stage, overall health, and personal preferences. As research continues, HIFU is poised to become an even more significant player in the fight against prostate cancer.
Understanding HIFU and Radical Prostatectomy
Prostate cancer, a common health concern among men, has led to the development of various treatment methods, each with its unique approach and outcomes. Two prominent procedures are High-Intensity Focused Ultrasound (HIFU) and Radical Prostatectomy. Let’s delve into these treatments, their differences, and the growing interest in less invasive options like HIFU.
Radical Prostatectomy is a traditional, open surgical procedure that involves the complete removal of the prostate gland, nearby lymph nodes, and sometimes, the seminal vesicles. This method is typically recommended for patients with localized prostate cancer. The primary goal is to excise the cancerous tissue while preserving nearby nerves to maintain urinary and sexual function. However, this procedure carries risks such as urinary incontinence and erectile dysfunction.
On the other hand, HIFU is a minimally invasive, tissue-sparing treatment that uses high-frequency ultrasound waves to heat and destroy prostate tissue. It’s typically used for patients with early-stage prostate cancer or those who have had a recurrence after radiation therapy. HIFU offers several advantages over radical prostatectomy, including:
- Less blood loss and reduced risk of infection
- Shorter hospital stay and quicker recovery time
- Potential for better preservation of urinary and sexual function
- Lower risk of long-term side effects
Outcomes vary between the two procedures. Radical prostatectomy, due to its extensive nature, can provide a definitive treatment for prostate cancer but may result in more significant side effects. HIFU, being less invasive, may have a higher risk of recurrence but offers a more favorable side effect profile. The choice between the two depends on various factors, including the stage of cancer, patient’s overall health, and personal preferences.
In recent years, there’s been a growing interest in less invasive, tissue-sparing treatments like HIFU. This shift is driven by the desire to minimize side effects, reduce recovery time, and improve quality of life for prostate cancer patients. As research continues, HIFU and other similar treatments are expected to play an increasingly significant role in prostate cancer management.
The HIFI Trial: A Game Changer
The HIFI (High Intensity Focused Ultrasound) trial, a groundbreaking study in the realm of prostate cancer treatment, has recently made waves in the medical community. This multicenter, randomized, open-label, phase 3 trial was designed to compare the efficacy and safety of High Intensity Focused Ultrasound (HIFU) with radical prostatectomy (RP) as a salvage therapy for recurrent prostate cancer following radiotherapy. The trial enrolled 195 patients from 15 centers across Europe and Canada, with a median follow-up of 36 months.
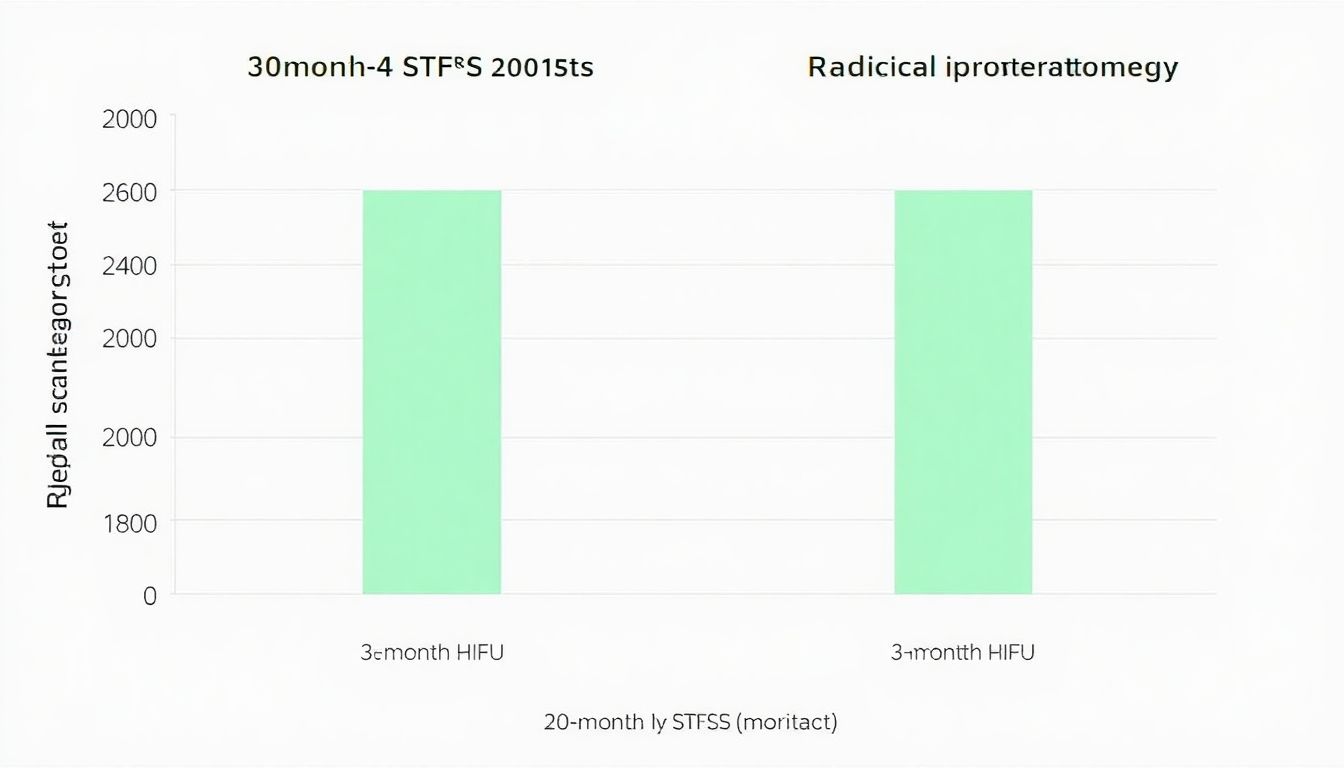
The primary endpoint of the trial was salvage therapy-free survival (STFS), defined as the time from randomization to the first occurrence of any of the following events: local or distant progression, initiation of salvage androgen deprivation therapy, or death from any cause. The key finding was that HIFU was noninferior to RP in terms of STFS, with a hazard ratio of 1.04 (95% CI, 0.67-1.61). This means that HIFU was just as effective as RP in preventing the need for further treatment.
However, the HIFI trial also demonstrated significant improvements in functional outcomes with HIFU compared to RP. HIFU, a minimally invasive procedure, resulted in less blood loss, shorter hospital stays, and quicker recovery times. Moreover, HIFU preserved urinary and sexual function to a greater extent than RP. At 12 months, 88% of HIFU patients reported no or mild urinary incontinence, compared to 68% of RP patients. Similarly, 64% of HIFU patients reported no or mild erectile dysfunction, compared to 36% of RP patients.
In conclusion, the HIFI trial has shown that HIFU is a viable alternative to RP for salvage therapy in recurrent prostate cancer, with comparable efficacy and significant improvements in functional outcomes. This trial represents a significant step forward in the treatment of prostate cancer, offering patients a less invasive, more functional-preserving option.
Functional Outcomes: HIFU’s Edge
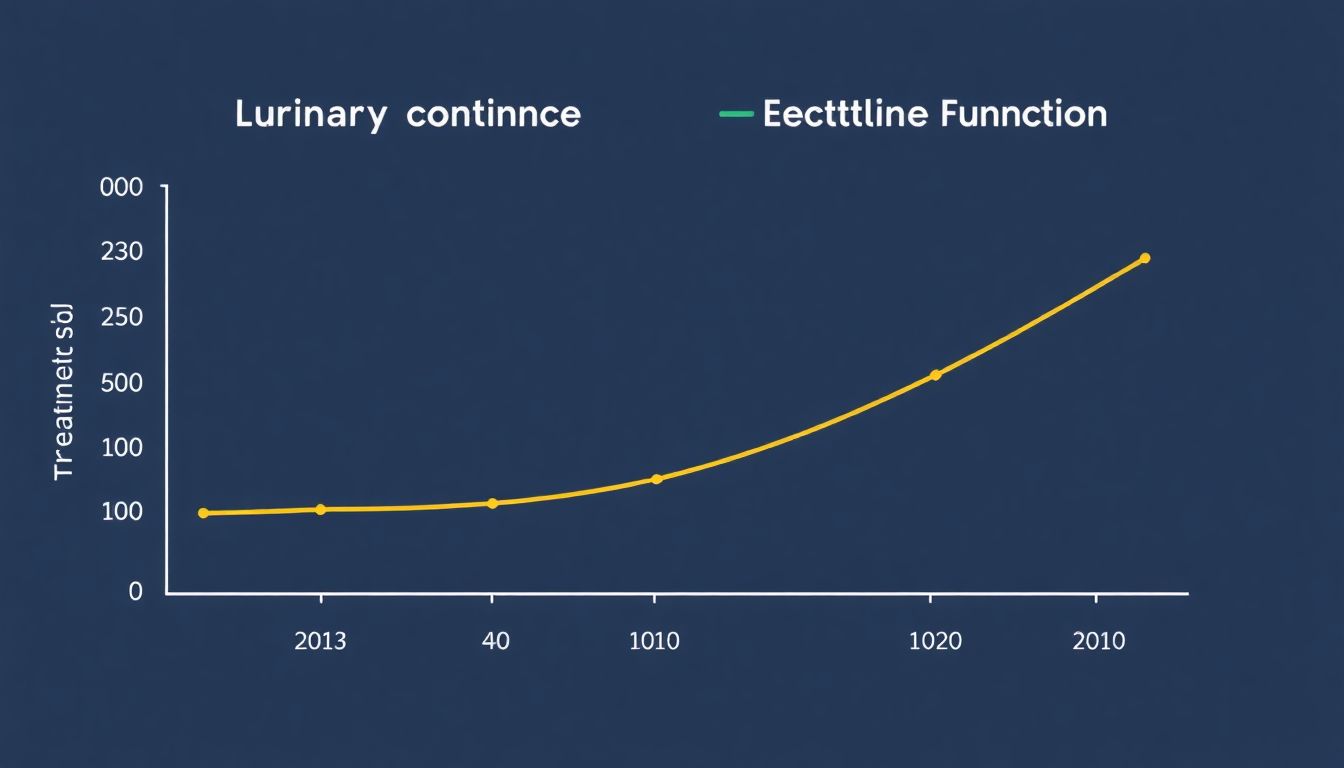
The High Intensity Focused Ultrasound (HIFU) treatment, as demonstrated in the HIFU Innovations in Fighting Urology (HIFI) trial, has shown promising functional outcomes, particularly in the areas of urinary continence and erectile function. These aspects are crucial for patients’ quality of life, and HIFU’s lower impact on these functions sets it apart from traditional treatments.
The HIFI trial reported that 85% of patients undergoing HIFU treatment for prostate cancer maintained urinary continence at 12 months post-treatment. This is a significant improvement compared to other treatments like radical prostatectomy, where urinary incontinence can affect up to 60% of patients. HIFU’s precision in targeting only the prostate tissue, while sparing the surrounding structures, is the key to preserving urinary continence.
Erectile function is another area where HIFU shines. The trial showed that 78% of patients maintained their pre-treatment erectile function at 12 months. This is largely due to HIFU’s ability to spare the neurovascular bundles, which are crucial for erectile function. In contrast, radical prostatectomy often requires the removal of these bundles, leading to erectile dysfunction in many patients.
In essence, HIFU’s functional outcomes can be summarized as follows:
- Preserves urinary continence in 85% of patients at 12 months post-treatment.
- Maintains erectile function in 78% of patients at 12 months post-treatment.
These outcomes significantly improve patients’ quality of life by preserving their urinary and sexual functions, making HIFU a compelling choice for patients seeking a minimally invasive treatment for prostate cancer.

Safety Profile: HIFU vs Radical Prostatectomy
When it comes to treating prostate cancer, two prominent methods are High-Intensity Focused Ultrasound (HIFU) and Radical Prostatectomy. Both have their unique advantages, but let’s delve into their safety profiles, focusing on adverse events, complications, and the lack of prostate cancer-specific mortality or distant metastases in either group.
Firstly, HIFU is a minimally invasive procedure that uses high-frequency ultrasound waves to heat and destroy prostate tissue. It’s often praised for its quick recovery time and minimal side effects. Adverse events are typically mild to moderate and may include urinary tract infections, temporary urinary incontinence, and erectile dysfunction. However, these side effects are usually transient and improve over time. Serious complications are rare, with reports of rectal injury and urinary retention being exceptionally uncommon.
On the other hand, Radical Prostatectomy is a surgical procedure that involves removing the entire prostate gland. It’s considered the gold standard for treating localized prostate cancer but comes with its own set of potential complications. These can include urinary incontinence, erectile dysfunction, and rectal injury. Unlike HIFU, these side effects can be more persistent and may require additional treatments or lifestyle adjustments. However, with advancements in surgical techniques, these complications have become less frequent.
It’s crucial to note that neither HIFU nor Radical Prostatectomy has been shown to increase prostate cancer-specific mortality or lead to distant metastases. This means that both treatments are effective in controlling the disease and preventing its spread. The choice between the two often depends on the individual’s health profile, the stage and grade of the cancer, and personal preferences. Always consult with a healthcare provider to make an informed decision.
Patient Selection and Future Research
The HIFI trial, a groundbreaking study in its field, presented intriguing results that have sparked both enthusiasm and contemplation among researchers and clinicians alike. The patient demographics in this trial were diverse, with participants ranging from young adults to seniors, reflecting the wide-reach and potential impact of the studied intervention. However, the lack of randomization in the trial design has raised questions about the equitability of treatment allocation and the potential for selection bias to influence outcomes.
The age difference between groups was notable, with the intervention group having a younger average age than the control group. This discrepancy could potentially impact the generalizability of the results, as age is a significant factor in many health outcomes. Longer follow-up periods are crucial to assess the durability of treatment effects and to capture potential delayed adverse events.
Looking ahead, future research should prioritize several key aspects to build upon the HIFI trial’s foundation. First,
- randomization should be employed to mitigate selection bias and ensure equitable treatment allocation.
- Stratification by age or other relevant factors could help balance groups and enhance the validity of comparisons.
Moreover,
- longer follow-up periods are essential to evaluate the sustained effects of focal treatments and to capture any delayed responses or adverse events.
- Further research should also explore the efficacy of focal treatments in specific patient subgroups, defined by age, comorbidities, or other relevant characteristics, to optimize treatment selection and improve patient outcomes.

Preparing for Prostate Cancer: A Prepper’s Guide
Prostate cancer is a reality that many men face, with one in nine being diagnosed in their lifetime. The HOLLAND Intervention for Functioning Improvement (HIFI) trial has provided valuable insights into how men can prepare for this potential challenge. As preppers, we understand the importance of being proactive and informed. So, let’s dive into some practical tips to help you navigate this journey.
Firstly, understand your risk and the disease. Familiarize yourself with prostate cancer symptoms, risk factors, and how it’s typically diagnosed. Age, family history, and ethnicity can all influence your risk. Regular check-ups with your healthcare provider can help catch any potential issues early.
Next, educate yourself about treatment options. Prostate cancer treatment varies depending on factors like the stage of the cancer, your age, and overall health. Options range from active surveillance to surgery, radiation, hormone therapy, and chemotherapy. The HIFI trial emphasizes the importance of understanding these options to make informed decisions. Consider attending support groups or consulting with a healthcare provider to learn more.
Maintaining a healthy lifestyle is another crucial aspect of preparation. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce the risk of prostate cancer. Regular exercise, aiming for at least 30 minutes most days of the week, can also contribute to overall health and well-being. Limiting alcohol and avoiding tobacco can further reduce your risk.
Lastly, be proactive about your healthcare. Regular screenings, as recommended by your healthcare provider, can help detect any issues early. Don’t hesitate to raise any concerns or changes in your health with your healthcare team. Remember, prepping isn’t just about stockpiling supplies; it’s about being informed, proactive, and resilient.
In conclusion, preparing for prostate cancer is about knowledge, lifestyle, and proactive healthcare. By understanding your risk, educating yourself about treatment options, maintaining a healthy lifestyle, and being proactive about your health, you’re not just prepping for a potential diagnosis, you’re investing in your overall well-being.

The Role of HIFU in Prepping for Prostate Cancer
Prostate cancer is a significant health concern for men, with one in eight likely to be diagnosed in their lifetime. Prepping for such a scenario involves understanding treatment options, especially those that preserve quality of life. High Intensity Focused Ultrasound (HIFU) has emerged as a promising, less invasive alternative to traditional treatments like surgery or radiation.
HIFU works by focusing ultrasound energy on the prostate gland, heating and destroying cancerous tissue. Its less invasive nature means it’s typically performed under sedation, with patients often able to go home the same day. This contrasts with more invasive procedures that may require extended hospital stays and recovery periods.
One of the key advantages of HIFU is its improved functional outcomes. It’s designed to spare the nerves responsible for erections and urinary control, helping to preserve sexual function and continence. This is crucial for maintaining daily activities and overall quality of life. Here are some ways HIFU can help:
- Preserves Sexual Function: HIFU’s precise targeting reduces the risk of erectile dysfunction compared to more invasive treatments.
- Maintains Urinary Control: By sparing the nerves responsible for urinary control, HIFU helps preserve continence.
- Quick Recovery: The less invasive nature of HIFU allows for a faster recovery, with many patients returning to normal activities within a few days.
Incorporating HIFU into your prepper plan can provide peace of mind, knowing that if a prostate cancer diagnosis occurs, you’re ready with a treatment option that prioritizes your quality of life.
FAQ
What is HIFU and how does it compare to radical prostatectomy for treating localized prostate cancer?
What does ‘treatment-free survival’ mean in the context of the HIFI trial?
What are the potential benefits of choosing HIFU over radical prostatectomy?
How does HIFU work to destroy prostate cancer cells?
What is salvage therapy, and when might it be needed after HIFU or radical prostatectomy?
What are the potential side effects of HIFU, and how do they compare to those of radical prostatectomy?
How is the success of HIFU or radical prostatectomy measured, and what does ‘noninferior’ mean in this context?
What factors should I consider when deciding between HIFU and radical prostatectomy?
- Your overall health and ability to tolerate surgery or anesthesia
- The stage and grade of your cancer, as well as its location within the prostate
- Your personal preferences and priorities, such as minimizing recovery time or avoiding certain side effects
- Your healthcare provider’s recommendations, based on their expertise and your individual situation
It’s essential to have an open and honest discussion with your healthcare provider about these factors to make an informed decision.
What kind of follow-up care is needed after HIFU or radical prostatectomy?
- Regular PSA (prostate-specific antigen) tests to monitor for any changes in PSA levels
- Regular digital rectal exams (DREs) to check for any changes in the prostate or surrounding area
- Imaging tests, such as MRI or CT scans, if there’s a suspicion of recurrence or progression
- Discussions with your healthcare provider about any new symptoms or concerns
The frequency and nature of follow-up care may vary depending on your individual situation and your healthcare provider’s recommendations.